Governor Gretchen Whitmer and her administration are selling a message of personal responsibility to curb the spread of COVID-19. In a recent interview on CNN’s “Inside Politics,” Lt. Gov. Garlin Gilchrist said, “we can vaccinate our way out of this pandemic.” But epidemiologists and public health experts say the state will struggle to outpace COVID variants without tightening restrictions.
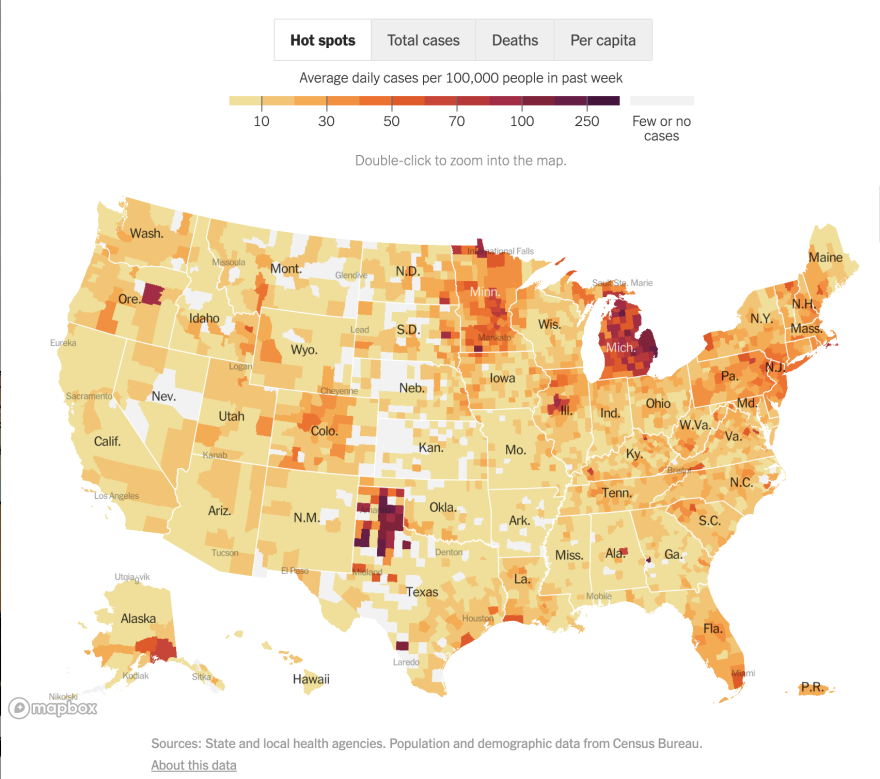
For the past few weeks, Michigan has had some of the highest rates of infection and hospitalization. Dr. Debra Furr-Holden, an epidemiologist and public health expert with Michigan State University, says Michigan’s bright red spot on a heat map of the nation has to do with a few factors: re-opening, vaccinations, and variants.
“Reopening did impact our spread, students went back to school, athletes engaged in sports, restaurants, bars, gyms, all of those things reopened,” Furr-Holden says. “It happened at the same time as this vaccination effort, but I don’t think we’ve taken into account adequately variants and the fact that variants are an unequal competitor for vaccines.”
The state reports around 40% of eligible Michiganders are fully or partially vaccinated, with more doses administered every day. But with the proliferation of variants such as B.1.1.7, and other possible variants native to Michigan, the role and timing of the vaccine in achieving herd immunity is hard to calculate.
“It looks like we’re winning because we’re vaccinating way more people than who are contracting the virus every day,” Furr-Holden says. “But think of the variants as having a jet pack. The virus has a jet pack and if you hit the jet pack on the virus, it can move much faster and cause a lot more infection, disability, and potentially death than will be prevented with the safe and very good vaccines.”
COVID-19’s novelty to humans makes it hard to know how it will mutate and what those changes will mean. The variants not only spread easier, but they could also make people sicker, which is “not a lesson we want to learn the hard way,” Furr-Holden says.
“This notion that we can get to herd immunity by combining natural immunity with vaccine-induced immunity is not good public health,” Furr-Holden says. “Public health is not about people getting sick. Public health is about preventing people from getting sick in the first place. And for us to do that well, we’ve got to give the vaccine a chance to be prevalent in the community and have the lion’s share of our population protected from infection.”
Furr-Holden says personal responsibility is important when it comes to preventing the spread of COVID-19. But, she says, without public health measures and restrictions in place at a critical moment such as this, the state could be caught in an ongoing “ebb and flow” of infection spikes.
“We saw early in the pandemic that hospital beds were full, all units were full, we were turning people away, we were rationing ventilators. We’re getting dangerously close to reaching that tipping point again,” Furr-Holden says. “If we don’t take these measures, predictably, that is where we will be and it won’t take very long, we’ll see that in the next few weeks.”
This article was written by Stateside production assistant Olive Scott.







